Gastroparesis: The causes, symptoms, and treatments for this little-known but serious gut paralysis condition

Studio Romantic // Shutterstock
Gastroparesis: The causes, symptoms, and treatments for this little-known but serious gut paralysis condition
woman indicating stomach pain to gastronenterologist
Whether you’re sorting out the symptoms of an undiagnosed condition or grappling with the weight of a recent diagnosis, gastroparesis can be a complicated and daunting disease to navigate. You’ll likely have questions about the condition, its implications, and the next steps forward.
To help you gain an understanding of gastroparesis, Guava Health compiled a list of frequently asked questions folks often have when it comes to outcomes and management.
![]()
Guava Health
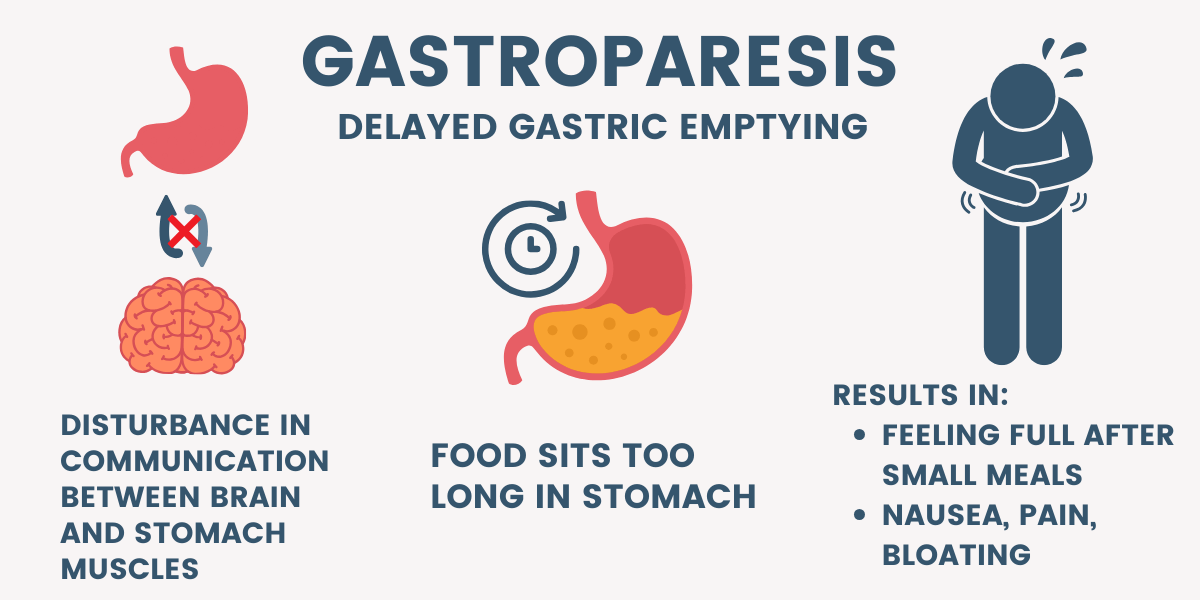
What is gastroparesis?
illustration showing steps to delayed gastric emptying
Gastroparesis is a condition that happens when your stomach muscles fail to contract normally, which can slow down or stop digestion altogether. This sort of gut paralysis is what leads to “delayed gastric emptying” and its accompanying symptoms.
What causes gastroparesis?
Gastroparesis occurs when the stomach’s normal muscular contractions, which help move food through the digestive system, are impaired. There are many reasons why this might happen, and sometimes doctors are unable to pinpoint one in particular (in which case it’s called idiopathic gastroparesis). However, some common factors that we know to be involved are:
1. Diabetes: High blood sugar levels over time can damage the vagus nerve and ‘pacemaker’ cells in the stomach muscles. This damage disrupts stomach muscle functions by interfering with normal nerve-to-stomach communication pathways.
2. Post-surgical complications: Surgeries involving the stomach or intestines can lead to nerve damage, triggering gastroparesis.
3. Infections: Certain viruses and bacterial infections can impact the nerves controlling stomach muscles, causing gastroparesis.
4. Connective tissue disorders: Hypermobility spectrum and connective tissue disorders like Ehlers-Danlos Syndrome (EDS or hEDS) are sometimes associated with minor gastroparesis, meaning slower digestion and delayed gastric emptying.
5. Nervous system diseases: Conditions like Parkinson’s disease, autonomic dysfunction, or multiple sclerosis can affect the nerves involved in digestion.
6. Medications: Some medications, like those affecting the nervous system (opiates, for example) and digestive systems, can contribute to delayed gastric emptying.
A couple of medications that have been recently associated with the onset of gastroparesis are those that contain semaglutide, like Wegovy and Ozempic. They’re meant for weight loss and work by slowing down digestion so that patients feel full longer, but in severe cases can cause gastroparesis.
Guava Health
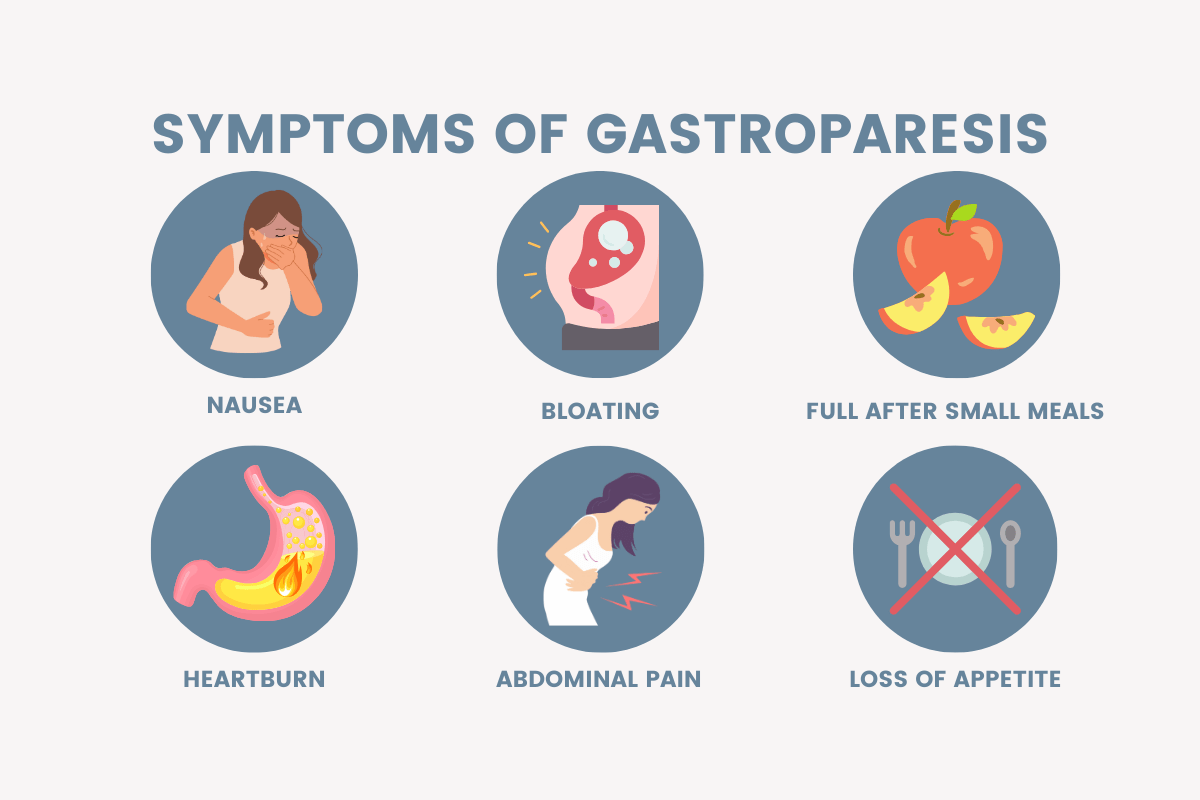
What are the symptoms of gastroparesis?
illustration of 6 common symptoms of gastroparesis
The most common symptoms of gastroparesis are nausea, vomiting, bloating, upper abdominal pain, and feeling full after small meals.
Is gastroparesis correlated with anorexia?
Gastroparesis and anorexia nervosa are two distinct illnesses, however, there is evidence of gastroparesis and gastrointestinal motility issues resulting from anorexia nervosa. Researchers suspect that malnutrition leads to muscular atrophy of the digestive tract and in turn, slower digestion and gastric emptying.
It’s important to note that gastroparesis is considered the far end of the spectrum in terms of stomach motility issues, so anorexia patients can experience these issues without obtaining a complete diagnosis.
How is gastroparesis diagnosed?
To test if your stomach isn’t digesting food fast enough, your doctor may perform what’s called a gastric emptying study. This involves keeping track of a tiny amount of radioactivity that you ingest before the test.
Imaging tests can also show any blockages that could be preventing proper digestion. A blockage rules out gastroparesis as a cause for the issue.
Which medications treat gastroparesis?
Medications for gastroparesis aim to manage symptoms and may include what are called prokinetic agents. These work by inducing stomach contractions to move food through your digestive tract. Two common ones are metoclopramide and domperidone.
Erythromycin is used to treat gastroparesis as well. Although it’s an antibiotic, it’s sometimes prescribed to stimulate stomach contractions.
To manage nausea and vomiting, antiemetics are also helpful, although they do not help with the digestive process.
For a comprehensive medication list, you can visit the National Institute of Diabetes and Digestive and Kidney Diseases.
What surgeries are there for gastroparesis?
If medications, lifestyle, and diet modification fail, you and your provider might consider surgical options for gastroparesis. Gastric electrical stimulation is the most common surgery for gastroparesis and uses small shocks to induce stomach contractions to move food along. Pyloroplasty is another option wherein the bottom part of the stomach is opened to allow the passage of food.
What’s the life expectancy for gastroparesis?
Gastroparesis itself does not typically affect life expectancy, although it does impact quality of life without proper treatment. There isn’t a specific death rate associated with gastroparesis, as there are plenty of resources for ensuring patients are properly nourished.
Guava Health
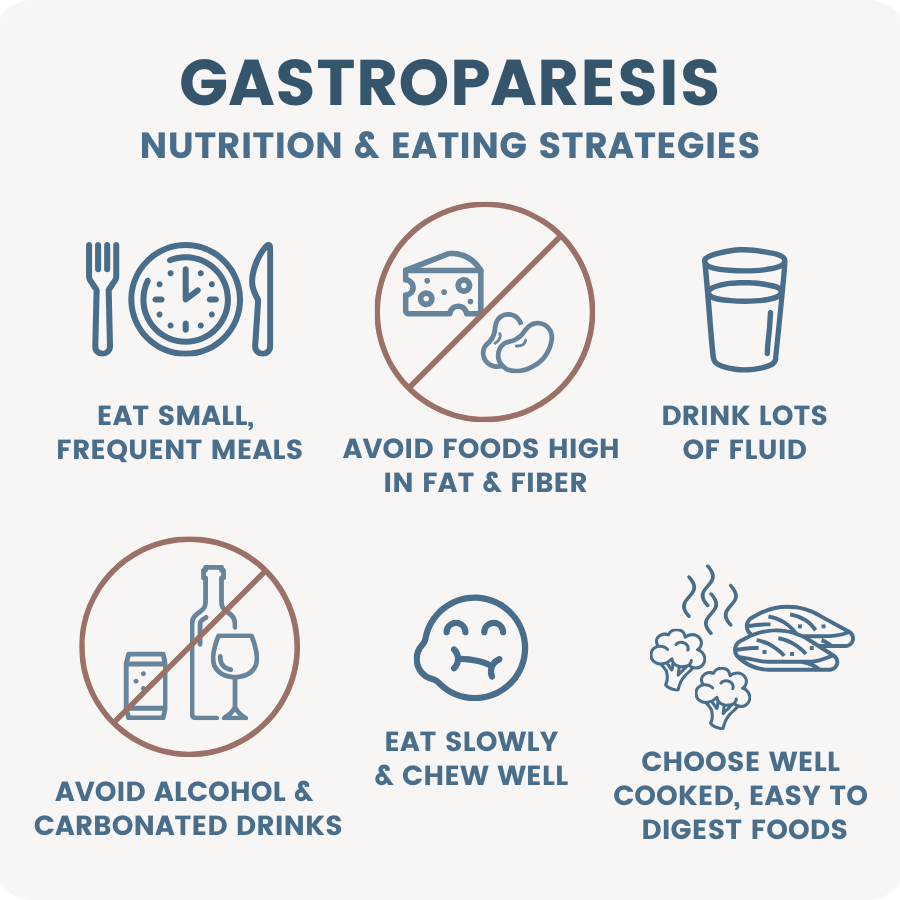
Is there a meal plan for gastroparesis?
illustration showing 6 things you can do to help symptoms
Yes, according to the International Foundation for Gastrointestinal Disorders, a gastroparesis-friendly meal plan involves consuming smaller, more frequent meals and avoiding certain foods that are hard to digest. A registered dietitian can create a personalized meal plan based on individual needs, considering dietary restrictions and preferences.
What are some tools to make daily life with gastroparesis easier?
There are a few worthwhile tools you might want to invest in if you’ve recently been diagnosed with gastroparesis. Here’s some to get you started:
1. Gastroparesis-friendly cookware: Purchase non-stick pans, blenders, and food processors for easy meal preparation.
2. Digestive supplements: You can try using supplements like ginger or herbal prokinetics to aid in the digestion of food and management of nausea, as recommended by healthcare professionals.
3. Pill organizers and medication reminders: Organize medications with pill organizers and set reminders for timely intake.
4. Wearable health trackers: Monitor overall health with devices tracking heart rate, blood sugar, sleep patterns, and activity levels to keep an eye on your daily patterns.
5. Food and symptom tracking apps: Use apps to track food intake, symptoms, and medication schedules for more organized management.
6. Educational Resources: It’s important to understand what’s happening in your body when you have gastroparesis. You can ask your healthcare provider for more information, as well as trustworthy websites. You should also stay informed about the relevant updates for treatment options, dietary modifications, and medications for gastroparesis.
Guava Health
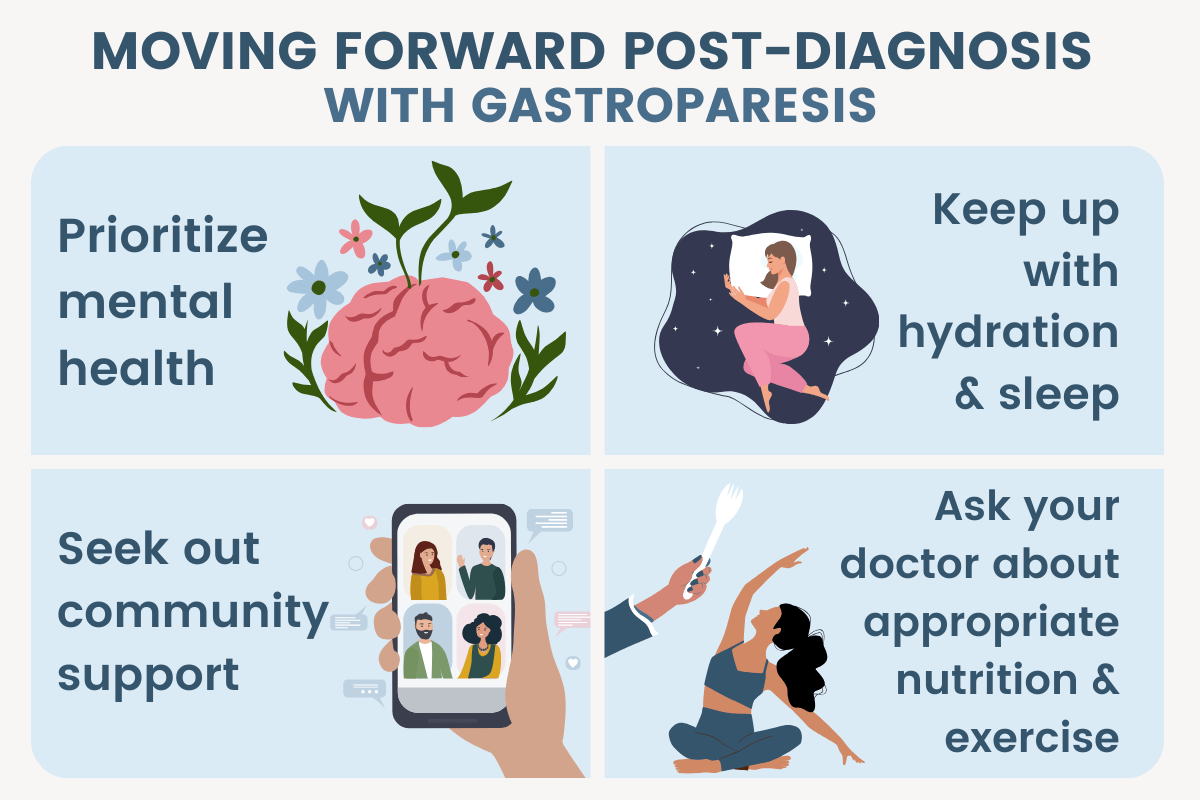
How do I start my ‘new normal’ with a gastroparesis diagnosis?
graphic showing 4 things to help move forward post-diagnosis
Getting diagnosed with gastroparesis can feel like a massive change to everyday life. The first step to starting your ‘new normal’ should be to understand what foods, medications, and treatments work for you.
This process will take time and energy, but the goal is to make you feel better in the long run. Prioritize your mental health by communicating with a therapist, friends, family, or your provider. Keep up with sleep, hydration, and appropriate exercise to manage your symptoms and flare-ups, and practice listening to what your body needs.
Remember that there are numerous gastroparesis communities and support groups that you can join as well. It’s incredibly beneficial to be able to ask questions and receive advice from those who understand your feelings.
I see a lot of people on social media with gastroparesis and feeding tubes. Will I have to get one too?
Feeding tubes, or enteral nutrition, are normally used in severe cases of gastroparesis, so your doctor will probably have you try out other treatment options first. However, if you’re super malnourished, dehydrated, or if other treatment options have failed, a feeding tube might be the best option to deliver the nutrients your body needs. How often you need it thereafter depends on your case severity, and a dietician can help you figure out an individualized plan.
If you do join the “tubie” community, remember that your feeding tube will get you feeling better, which is the most important part of your treatment. There are also tons of support groups for patients in your position who can offer understanding and advice.
This story was produced by Guava Health and reviewed and distributed by Stacker Media.