New laws are increasing price transparency in health care. Here's what they mean for you.

Canva
New laws are increasing price transparency in health care. Here’s what they mean for you.
A stethoscope sitting on top of a medical bill.
Health care is one of the most burdensome expenses saddled on Americans. Half of adults in the U.S. report struggling to afford health care, and about the same portion says a $500 medical expense would push them into debt. A quarter of adults put off getting the care they need because of that financial cost, according to surveys from KFF, the organization formerly known as the Kaiser Family Foundation.
What’s more, being insured often isn’t enough to soften the blow. The majority of people in medical debt today actually have health insurance, medical billing analysts report.
Workers and employers have seen their costs for health insurance plans rise significantly since the pandemic began in 2020, a trend that had already been playing out long before. Costs are projected to rise another 6.5% in 2024, according to benefits consulting firm Willis Towers Watson. Rising drug costs, a growing elderly population, pent-up demand post-pandemic, shortages of care workers, and expensive technologies all factor into the increasing expense of health care.
A slew of new rules has been signed into law in the last several years to help Americans, as well as the publicly funded Medicare and Medicaid programs, save money on health care expenses. Broadly, the new laws pertain to prescription costs, price negotiations, surprise billing, and cost transparency. These measures have largely been championed by politicians on both sides of the aisle.
Care Better analyzed information from the Centers for Medicare & Medicaid Services and major hospital systems to compile this explanation of what Americans can expect from new health care cost transparency laws.
The Trump administration previously enacted rules through executive order requiring hospitals to publicly post the costs of certain services online and another that requires health insurers to share the costs of services covered under their health care plans, which was rolled out in phases under the Biden administration.
A study from the University of Minnesota published in 2023 estimated that price transparency rules for health plans alone could lead to “substantial savings,” potentially in the tens of billions of dollars, benefiting consumers, employers, and even insurers.
The most recent effort to boost health care transparency is making its way through Congress this winter. It’s H.R. 5378, nicknamed the Lower Costs, More Transparency Act. The resolution was voted through the House of Representatives in December and now awaits consideration from the Senate.
The bill is an amalgamation of many existing draft bills championed by Republican and Democratic Congress members who argue the new resolution will empower consumers to make informed decisions related to their health care, lower drug costs, and end overcharging for services by hospitals. It would build on previous transparency measures enacted prior to the pandemic. Health care executives and for-profit hospitals have been critics of the legislation, arguing the changes to Medicare reimbursements will hurt hospitals, particularly those in rural areas where consumers have few other options for care.
Read on to learn more about the changes that could be coming if the Lower Costs, More Transparency Act becomes law.
![]()

Canva
Site-neutral procedures for Medicare
Two female health care professionals looking at X-rays.
Implementing what are known as “site-neutral” procedures for Medicare is one area that hospital executives have pushed back against in particular. This part of the legislation would make it so that hospitals can’t charge Medicare more for the same procedures and services provided at lower expense to the program by physicians’ offices. A 2021 estimate by the nonpartisan Committee for a Responsible Federal Budget organization projected that eliminating the cost of the unequal charges at hospitals could save Medicare more than $150 billion by 2030.

Canva
Spread pricing under Medicaid is out
An older African American man holding a bottle of medication in a pharmacy.
Spread pricing is a practice where pharmacy benefit managers—some of the most recognizable names being CVS Caremark and OptumRx—charge Medicare or Medicaid more for a drug than it was charged by the pharmacy. Studies have highlighted the potential for the practice to be very profitable for the organizations charged with negotiating drug prices for health plans. The new resolution would ban the practice under Medicaid reimbursement.
Canva
Hospital price transparency
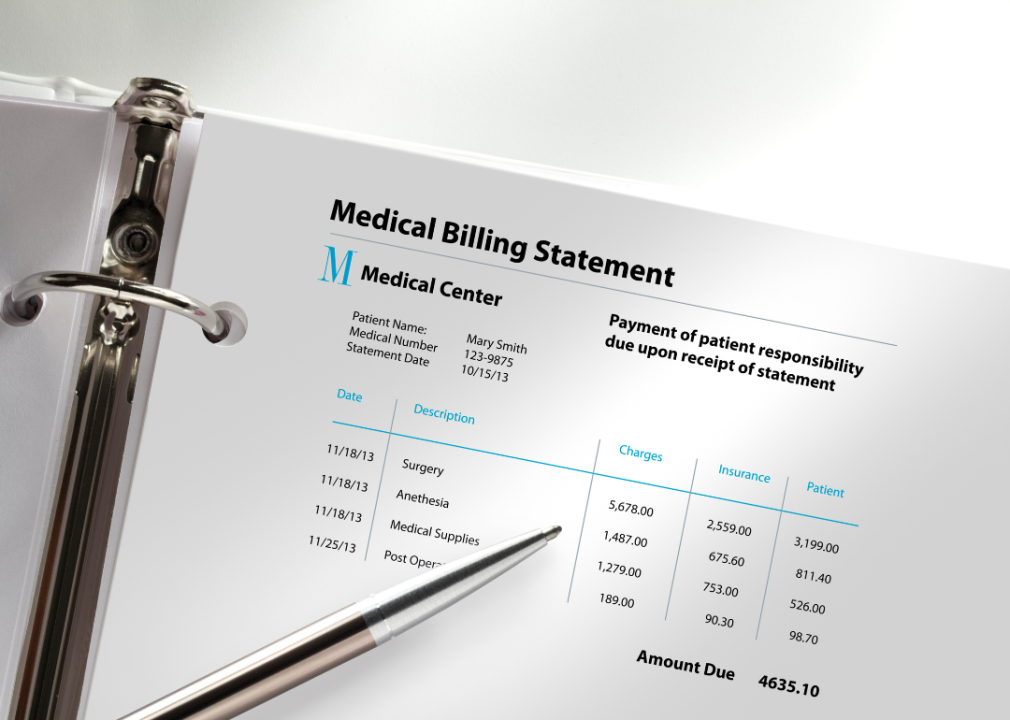
A closeup of a page of a medical bill in a folder.
All hospitals would be required to make public the cash and insurance-adjusted costs of at least 300 health care services. It also requires them to provide those prices in a single file that can be read by popular programs so that entrepreneurs might be able to develop shopping services for consumers, promoting healthy competition among health care providers. Studies show that compliance rates for existing rules are low, and hospitals are struggling to get in compliance due to a lack of standardization, according to KFF.

Canva
Public lab test and imaging pricing
An African American female holding a blood sample in a lab.
Part of the proposed resolution would require diagnostic labs to publish the cash costs of specific clinical tests as well as the minimum and maximum insurer-negotiated rates under Medicare and Medicaid. Imaging services like MRIs and X-rays would be subject to similar requirements.

Canva
Additional funding for health care worker training programs
Two female young nurses and two young male nurses in a circle listening to the nurse talking to them.
The resolution would also add around $5 billion in funding for programs that work to expand the pipeline of professionals going into health care careers. The Health Resources & Services Administration estimates that in regions of the U.S. deemed Health Professional Shortage Areas by the federal government, the public needs nearly 13,000 more primary care practitioners, almost 10,000 dental health care workers, and more than 6,000 mental health practitioners. The shortage of workers isn’t just about making services easier to access; it’s partly responsible for higher health care costs for consumers, studies have found.

Canva
Extending the ban on pharmacist gag clauses
A closeup of hands writing holding a pen and two orange bottles of medication on the table.
Private health insurance plans use legal agreements known as “gag clauses” to prevent pharmacists from disclosing when a cheaper drug is available to a patient. The resolution would clarify earlier rules so that the ban on these clauses applies to all private health insurance plans.

Canva
Health care coverage price transparency
A stethoscope sitting on top of health insurance benefits document.
Similar to hospital transparency rules, the resolution also builds on previous efforts to require health care plans to be transparent about the rates they charge for in-network and out-of-network services as well as prescription drugs. The price info shared would also have to be posted in an accessible, machine-readable file.
Story editing by Ashleigh Graf. Copy editing by Tim Bruns. Photo selection by Ania Antecka.
This story originally appeared on Care Better and was produced and
distributed in partnership with Stacker Studio.