10 states haven't expanded Medicaid—here are the health care challenges they face
Image Point Fr // Shutterstock
10 states haven’t expanded Medicaid—here are the health care challenges they face
Man in consultation with a doctor.
The 2010 Affordable Care Act offered states an opportunity to expand eligibility for Medicaid, a health care program paid for jointly by the federal and state governments that covers care for low-income children, adults, people who are pregnant or have a disability, and older adults.
The expansion extended Medicaid coverage to all low-income adults earning up to 138% of the federal poverty level—for individuals, that’s roughly $20,120 in 2023. To cover the costs, the federal government would pay for 90% of the program, and states would have to pay the remaining 10%.
The result was a significant increase in the number of people covered by Medicaid. Before the expansion, 56.5 million people were enrolled in Medicaid and the closely associated Children’s Health Insurance Program. By May 2023, those programs enrolled 93.8 million people, according to the Kaiser Family Foundation. That’s 1 in 5 people (and 4 in 10 children) in the United States.
Under the original law, states that chose not to expand their eligibility criteria would risk not receiving any federal funding for any of their Medicaid programs. But in 2012, the Supreme Court overturned that penalty for not expanding eligibility, and made it fully optional for states.
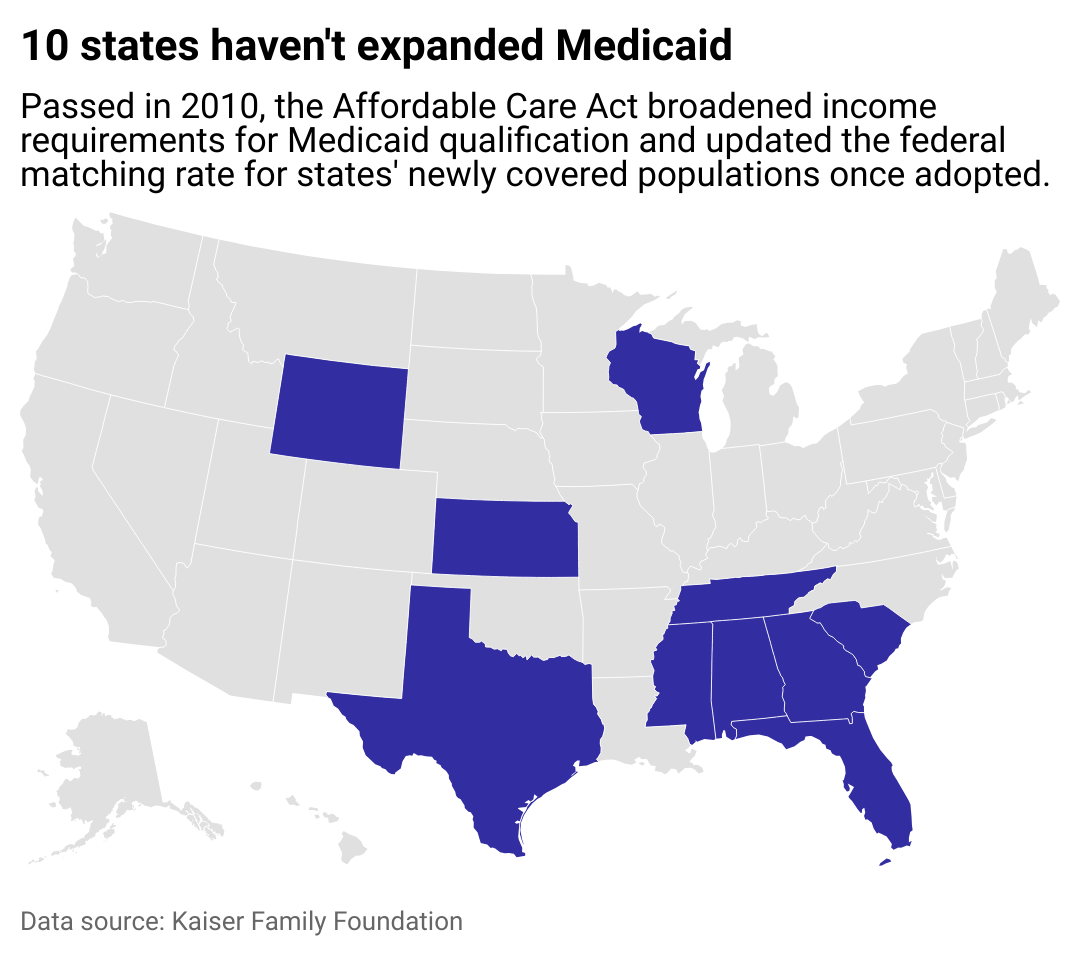
While 40 states and Washington D.C. have adopted expansion, 10 have not. Most states that haven’t expanded have less health care coverage than the national average.
Foothold Technology used data from the Kaiser Family Foundation to look closer at each of the 10 states that haven’t expanded Medicaid to learn about their ongoing health care challenges. Data points on Medicaid and Children’s Health Insurance Program enrollment are also included. The difference in enrollment from before the Affordable Care Act compared to May 2023 is calculated based on total enrollment per 100 residents in the state.
![]()
Foothold Technology
Where Medicaid expansion hasn’t been adopted
Map showing the 10 states which haven’t expanded Medicaid. Passed in 2010, the Affordable Care Act broadened income requirements for Medicaid qualification and updated the federal matching rate for states’ newly covered populations once adopted.
At the beginning of 2014, 24 states and Washington D.C. expanded their coverage immediately. Since then, another 16 states have followed suit. In March 2023, North Carolina became the most recent state to enact Medicaid expansion legislation, but implementation may not come until 2024.
In the remaining states, the Kaiser Family Foundation estimates that 1.9 million people who earn too much to receive government subsidies to buy private health insurance would be covered by Medicaid if it were expanded. States that haven’t adopted expansion cite economic factors and federal governmental overreach as reasons why they won’t. But Kaiser reviews of studies on Medicaid expansion have found people in states that did expand eligibility have better health, which is good for the states’ health care providers and overall economies.
CGN089 // Shutterstock
Alabama
Patient’s hand with an attached pulse oximeter on finger for monitoring.
– Medicaid and CHIP enrollment, May 2023: 1.2 million (23.7 per 100 people, 18.6% below national average)
– 43.4% increase in enrollment from before Affordable Care Act
Alabama ranks 42nd in the nation in terms of overall health system performance, according to the Commonwealth Fund. Heart disease is the state’s leading cause of death and the state has the third-highest heart disease death rate in the nation, with 247.5 deaths per 100,000 people, according to the Centers for Disease Control and Prevention. Some experts say this rate doesn’t have to be so high—in 2021, the Cleveland Clinic found that 90% of heart disease cases could be prevented through diet, exercise, and not smoking.
To combat the state’s health challenges, the University of Alabama at Birmingham launched a public-private partnership called Live HealthSmart Alabama in 2019. The organization provides mobile health screenings and produce markets, accessible physical activities, and health and wellness education.
Gligatron // Shutterstock
Florida
Happy senior woman having blood pressure test performed by a doctor.
– Medicaid and CHIP enrollment, May 2023: 4.8 million (21.4 per 100 people, 31.8% below national average)
– 13.0% increase in enrollment from before Affordable Care Act
When pandemic-related Medicaid protections ended in early 2023, about 900,000 Floridians were dropped from Medicaid rolls, a total that could climb to 1.5 million, according to NPR. This could cause 388,000 citizens to lose not only their health coverage but also any government aid to purchase a new insurance plan, according to Kaiser.
The state developed a State Health Improvement Plan for 2022-2026 to focus on seven health concerns and partner with local organizations to tackle them. These priority areas include Alzheimer’s and dementia, chronic diseases, maternal and child health, mental health and substance abuse, injury and violence prevention, and transmissible diseases. The plan also seeks to address social and economic barriers to good health, with goals to expand education, improve access to services, and promote healthy lifestyles.
Medical-R // Shutterstock
Georgia
Blurred image of patients in a hospital waiting room.
– Medicaid and CHIP enrollment, May 2023: 2.5 million (23.2 per 100 people, 21.3% below national average)
– 50.8% increase in enrollment from before Affordable Care Act
In July 2023, Georgia’s Department of Community Health launched Georgia Pathways to Coverage, an expansion of Medicaid coverage for uninsured low-income adults aged 19 to 64. The program comes with the requirement that citizens have a job, take job training, or participate in community service, or are going to school at least part-time for at least 80 hours per month. This caveat makes Georgia the only state to have a work mandate for this Medicaid program.
Georgia’s program does not qualify for federal funding, so the state will be paying $2,490 per enrollee versus $496 if the state had implemented Medicaid expansion, according to CNN. The state says it has budgeted for 100,000 enrollees in the first year, although it had approved only 265 applications in its first month, ABC News reported.
Dragana Gordic // Shutterstock
Kansas
Close up of a Psychologist holding hands of a female patient.
– Medicaid and CHIP enrollment, May 2023: 472,492 (16.1 per 100 people, 75.0% below national average)
– 23.1% increase in enrollment from before Affordable Care Act
If Kansas Gov. Laura Kelly—a Democrat—had her way, the state would already have adopted Medicaid expansion. However, a Republican-led state legislature did not include her proposal in its fiscal year 2023 budget and also didn’t take up an expansion bill she introduced. In June 2023, the governor again called for expansion, citing the state’s need for increased mental health coverage.
Kansas ranks last in the country for prevalence of mental illness and access to care, according to a 2023 report by Mental Health America. The governor says that expanding Medicaid would provide affordable mental health and substance abuse treatment to 150,000 more Kansans, of whom one-third are already in need of those services.
Sopotnicki // Shutterstock
Mississippi
Newborn baby in a small hospital bed.
– Medicaid and CHIP enrollment, May 2023: 791,409 (26.9 per 100 people, 4.6% below national average)
– 30.7% increase in enrollment from before Affordable Care Act
The fact that Mississippi has not adopted Medicaid expansion may not be a surprise. When the federal Medicaid program was enacted in 1965, Mississippi didn’t implement it until 1969—and was one of the last states to do so. The state legislature argues against expansion on the grounds that it would be too expensive to implement.
Mississippi struggles with health care—it ranks last in the nation for health system performance, according to the Commonwealth Fund. The state has low marks for preterm birth rates as well as deaths from breast and cervical cancer. It also ranks last in premature deaths from treatable causes and second-to-last for premature deaths from preventable causes.
Ground Picture // Shutterstock
South Carolina
Doctor presenting results to a patient with an oxygen mask and his wife.
– Medicaid and CHIP enrollment, May 2023: 1.3 million (25.1 per 100 people, 12.3% below national average)
– 34.2% increase in enrollment from before Affordable Care Act
In South Carolina, Medicaid covers 1 in 8 adults aged 19 to 64 and 47% of births. The state has committed to some extension of the program, specifically 12-month postpartum coverage.
Health care is a challenge in South Carolina, as 6 in 10 adults have at least one chronic disease, and 4 in 10 have more than one, according to the South Carolina Department of Health and Environmental Control. Chronic diseases, including heart disease, diabetes, stroke, and cancer, account for nearly 57% of deaths in the state. In response, Clemson University and the Medical University of South Carolina have partnered for an initiative called Healthy Me—Healthy SC that provides educational programs, health screenings, vaccinations, a mother’s milk bank, and a pain rehab program.
Tada Images // Shutterstock
Tennessee
Closeup of the homepage of Medicaid.gov seen on a smartphone.
– Medicaid and CHIP enrollment, May 2023: 1.8 million (25.7 per 100 people, 9.5% below national average)
– 34.1% increase in enrollment from before Affordable Care Act
Tennessee is ranked 46th in the nation for health care, earning low marks for avoidable emergency-room visits and premature deaths from treatable or preventable causes, according to the Commonwealth Fund.
The state’s mainly rural geography—78 of its 95 counties are rural—suffers from a lack of health care opportunities. Since 2010, 13 of 16 hospital closures in the state have been in rural areas. To reach people in those areas, the University of Tennessee Health Science Center launched a mobile health unit in June 2023 that can provide primary care, prenatal care, mental health care, chronic disease management, and HIV care services.
Rawpixel.com // Shutterstock
Texas
Nurse making the bed at a hospital.
– Medicaid and CHIP enrollment, May 2023: 6.0 million (19.8 per 100 people, 41.8% below national average)
– 25.0% increase in enrollment from before Affordable Care Act
In 2022, about 1 in 6 Texans were uninsured, representing the highest rate in the nation, according to the Census Bureau. However, that rate may rise again as pandemic-related protections for Medicaid recipients expire. Over 500,000 people have lost Medicaid coverage since April 2023, according to the Texas Tribune.
The state government will likely not enact a plan anytime soon. Although 69% of Texans support Medicaid expansion, some state leaders, including Gov. Greg Abbott and Lt. Gov. Dan Patrick, are opposed to the program, despite the fact that the state could receive as much as $5.4 billion in federal aid to help fund it.
Rawpixel.com // Shutterstock
Wisconsin
Baby at a visit with a doctor.
– Medicaid and CHIP enrollment, May 2023: 1.5 million (24.6 per 100 people, 14.2% below national average)
– 43.4% increase in enrollment from before Affordable Care Act
Wisconsin is the only state in the Great Lakes region that hasn’t signed on to Medicaid expansion, but Democratic Gov. Tony Evers is trying. Evers included Medicaid expansion in his 2023-2024 state budget proposal, but the state legislature’s Joint Finance Committee voted to remove it.
Wisconsin ranks 49th in terms of public health funding—its $72 per capita is $44 less than the national average, according to United Health Foundation. The state faces challenges with excessive drinking and fentanyl overdoses, and people of color have disproportionate numbers of lower birth-weight babies compared to white residents.
Andrey_Popov // Shutterstock
Wyoming
Close-up of a doctor measuring a patient’s blood pressure with a stethoscope.
– Medicaid and CHIP enrollment, May 2023: 84,685 (14.6 per 100 people, 93.2% below national average)
– 25.6% increase in enrollment from before Affordable Care Act
Medicaid covers 1 in 14 adults and 1 in 4 children in Wyoming, according to the Kaiser analysis. Expansion would provide an additional 15,200 people the opportunity to have health coverage, 6 in 10 of whom live below the poverty line but don’t currently qualify for help.
In 2021, state legislators started introducing bills to implement the expansion, but the bills died for three subsequent years, even though the state’s population is in favor of it, according to Wyoming Public Radio. The state’s aging population has challenges with chronic diseases. For instance, more than 2 in 5 adults aged 65 and older have high blood pressure, the 2023 Wyoming Healthy Aging Data Report found.
Data reporting by Emma Rubin. Story editing by Jeff Inglis. Copy editing by Tim Bruns. Photo selection by Clarese Moller.
This story originally appeared on Foothold Technology and was produced and
distributed in partnership with Stacker Studio.










