New study finds that brain structure changes cyclically throughout the menstrual cycle
Guava Health
New study finds that brain structure changes cyclically throughout the menstrual cycle
An illustration showing different colored lines connecting each side of the brain.
Is it your understanding that only hormone levels fluctuate throughout the menstrual cycle? Well, this news might change your mind. Hormones aren’t the only bodily component that follows a monthly rhythm.
In October 2023, a research study out of the University of California, Santa Barbara (UCSB) found that the entirety of womens’ brain structure actually fluctuates throughout the menstrual cycle as well. For this report, Guava Health interviewed Elizabeth Rizor, a dedicated PhD student who worked on this study.
Rizor shared a rare glimpse into this relationship between hormonal health and brain structure. How this research could redefine the current understanding of womens’ health in areas like menstrual symptoms and exercise were also discussed.
To start, Rizor explained the body parts and processes that were tracked — specifically brain matter and the female hormonal cycle.
![]()
Guava Health
There’s lots of gray area in the brain — but even more white area
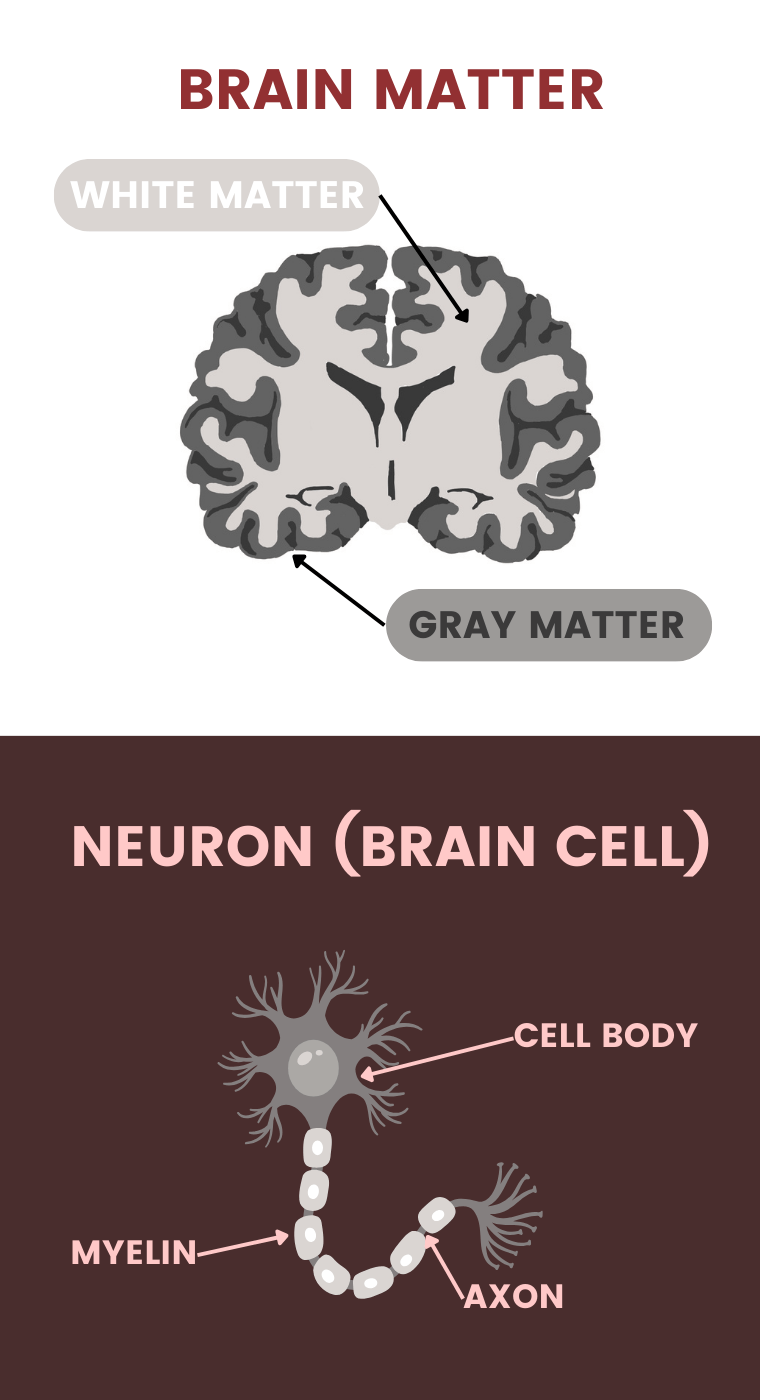
An illustration of the brain matter showing the white and grey part, including the parts of a neuron.
The building blocks of our brains are gray and white matter. Gray matter is typically where most of the focus goes, since it’s responsible for daily functions like controlling movement, memory, and emotions. Gray matter is the outer layer of the brain, and as Rizor described, “is like a cortical ribbon that goes along the edge of the brain. Gray matter is where functional activation is happening. It’s where the cell bodies [of brain cells or neurons] are really clustered.”
About 40% of the brain is gray matter, while the other 60% is white matter. If white matter makes up over half of our brain, then it must also have a pretty important role.
Why is white matter white? Myelin wraps around the axons of brain cells, which are the long cable-like connections between cell bodies. Myelin helps speed up the rate that electrical signals travel across the brain. When white matter is compromised, this can affect sensory, motor, and cognitive functions (basically the ability to sense, move, and think).
Rizor described white matter to be “fatty tissue underneath the outer layer of gray matter that consists of bundles of axons. You can think of it kind of like bundles of straws, or highways that transmit information between the different brain regions in the gray matter. It can perform this long-range cross-communication between different areas in the brain.”
It seems that white matter is the vital medium for messages to be sent across different parts of the brain. If these areas are changing, this could imply changes in communication. The potential impact of this on womens’ cognition, emotion, and overall brain function is still being investigated.
What has been observed is that white matter changes across hormonal transition phases like puberty, taking birth control, menopausal treatment, and gender transition treatment — however, there is a lack of research exploring standard, baseline hormonal and brain changes across a natural menstrual cycle.
Rizor and her colleagues noticed this lack of research in naturally cycling young women. Women make up half of the population, and nearly all women naturally cycle for decades of their lives. Discoveries related to this brain-hormone connection have implications for a drastic portion of the population.
Guava Health
Studying 30 women under age 30
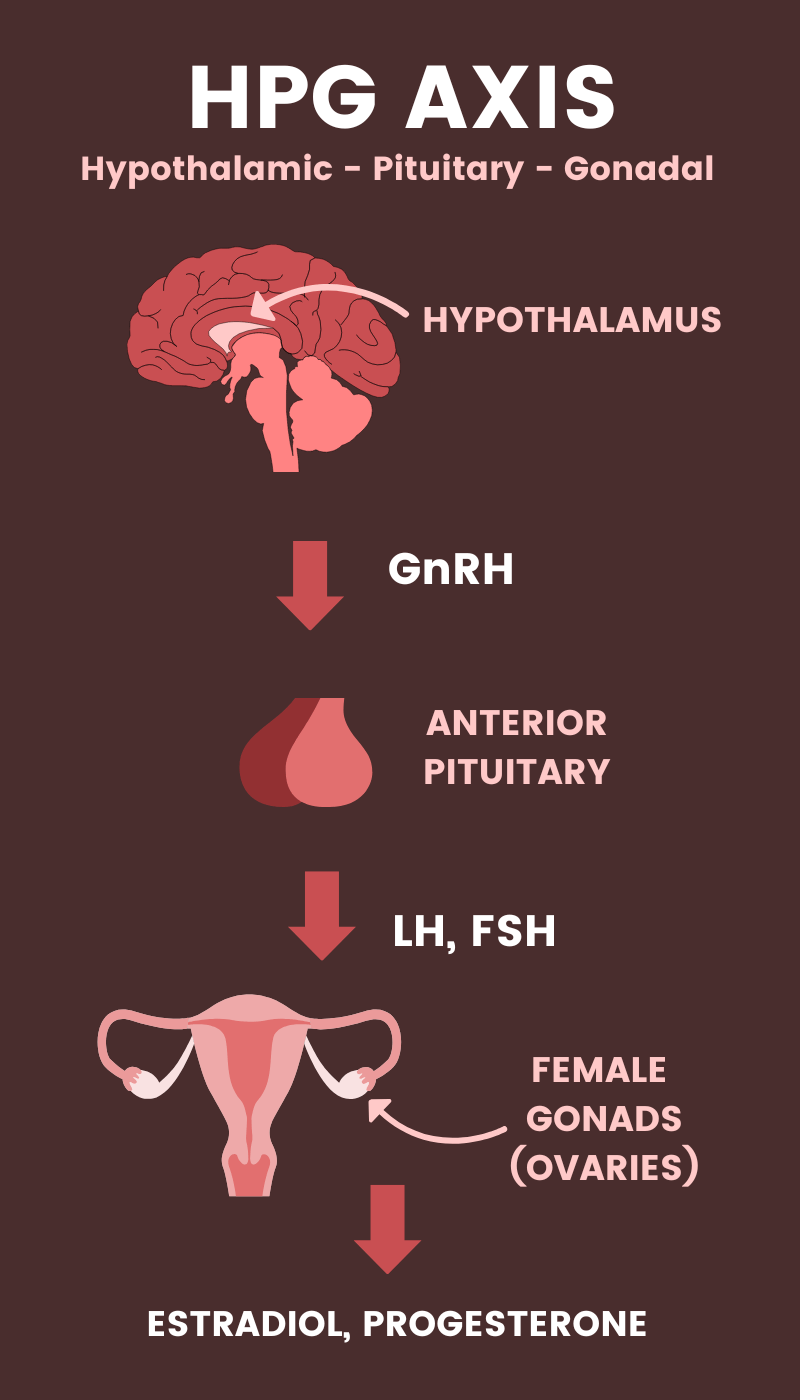
An illustration showing the HPG axis.
The UCSB study included 30 women ranging between 18 to 29 years old (21 being the average). The average length of these womens’ cycles was 31 days.
The hormones researchers tracked are a part of the HPG axis — HPG stands for Hypothalamic – Pituitary – Gonadal, and axis refers to how these organs span across the body. Brain scans and hormone levels were analyzed at three points throughout the menstrual cycle: Menses, Ovulation, and Mid-Luteal.
After all of the brain scans and blood tests were collected, the researchers found that follicle stimulating hormone (FSH) and progesterone had a see-saw relationship. FSH had moderate levels during menses and was high during ovulation. Progesterone was higher during the luteal phase, which is the other end of the cycle. This didn’t surprise the researchers.
However the big shocker, as Rizor explained, was that “both white matter and gray matter had an opposing tension between the two hormones, where one [hormone] was correlated with change in white matter, and the other correlated with the opposite. The same occurred in the gray matter and cortical thickness [width of gray matter cortical ribbon] as well.”
Guava Health
What’s the impact of this?
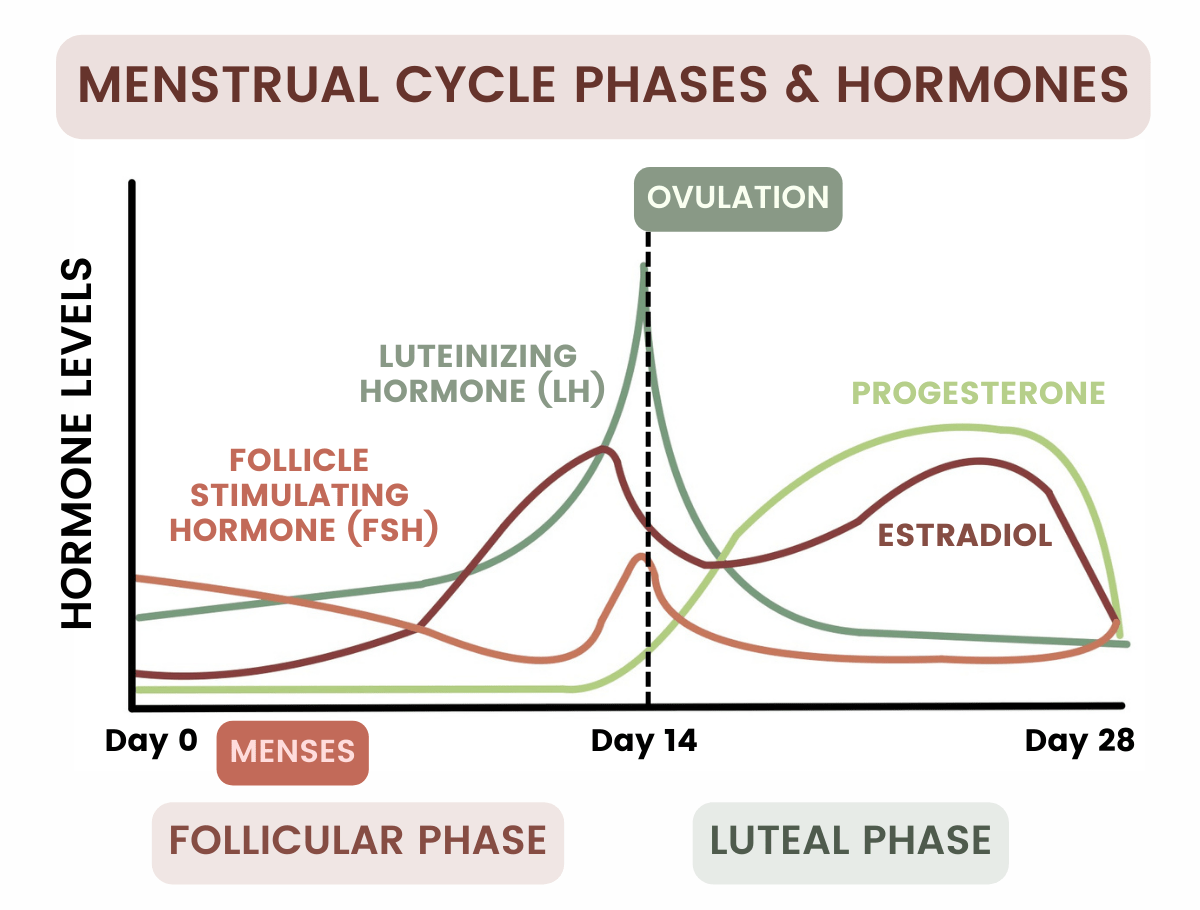
A graph showing menstrual cycle phases and hormones.
While this study didn’t explore brain structure impact on cognition across the cycle, the cyclical changes in brain matter may infer cognitive advantages for one phase versus another. Phase-dependent brain changes could also provide explanations for differences in emotional processing, cognitive performance, and motivation throughout the menstrual cycle that are worth future investigation.
More and more research has found differences in attention, memory, and verbal and spatial skills throughout the cycle. However, studies on premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) have only looked into changes in executive function and attention.
This work can be used as a baseline in furthering our understanding of menstrual disorders such as PMS and PMDD. Some women with these disorders have reported “difficulty concentrating and impaired work productivity” during the late luteal phase.
More and more research has found differences in attention, memory, and verbal and spatial skills throughout the cycle. However, studies on PMS and PMDD have only looked into changes in executive function and attention.
Executive function is how thoughts, emotions, and actions are managed and controlled. This aspect of the brain allows for planning, achieving, and problem-solving. If there is a change in these functions, the ability to perform daily activities could be affected.
How do these brain and hormonal changes affect menstrual symptoms?
When asked if there were findings from the study that surprised her, Rizor said, “For some of the individual findings, you can see some people trend opposite of the group.”
This observation reveals that biometrics and symptoms don’t always align with what is considered “normal”. As Rizor said, “Everyone has different emotional and cognitive experiences. There’s a lot of individual differences throughout your experience of the cycle and hormone fluctuation.”
However, if you think you might have PMDD or other menstrual difficulties, the consultation of healthcare professionals is advised to evaluate whether you are suffering from deeper brain or hormonal imbalances. The symptoms you experience are worth paying attention to, not just ignoring or suppressing.
Rizor shared personally about her own experience as a naturally cycling woman and the pressure she felt from herself and others to ignore her cycle symptoms:
“Throughout my life, I didn’t think critically often enough about my menstrual cycle, just that it was a kind of nuisance I had to deal with. I also felt pressure to stay normal and perform the same every single day. What I think our study does well, as do some other studies, is that it literally shows there are baseline anatomical changes that are fairly consistent across a group of around 30 women.”
And, these changes do not exist in isolation.
Rizor went on to say, “These hormones are circulating in the blood throughout your entire body, so they’re not just going to be affecting your reproductive organs, or your abdomen. These hormones cross the blood brain barrier, going into the brain. There could be other effects on other organs as well — so it’s really a whole body process.”
There is reassurance in remembering that women don’t have to feel alone in their experiences — tuning in and recognizing symptoms can provide opportunities to connect with others. There is no shame in experiencing these symptoms. The task is to figure out how to understand these changes to figure out what your bodies are telling you.
“We can all experience our own symptoms and be used to having them in our day-to-day lives. On certain days during my PMS phase, I get more moody and bloated. But I think we often feel that we’re so individual and alone in our experiences. But you don’t actually know — if you don’t talk about it — what other people are also experiencing. You might not make the link that these things are happening because of baseline biological processes,” Rizor said.
Guava Health
How do changing brain and hormonal changes influence exercise routines?
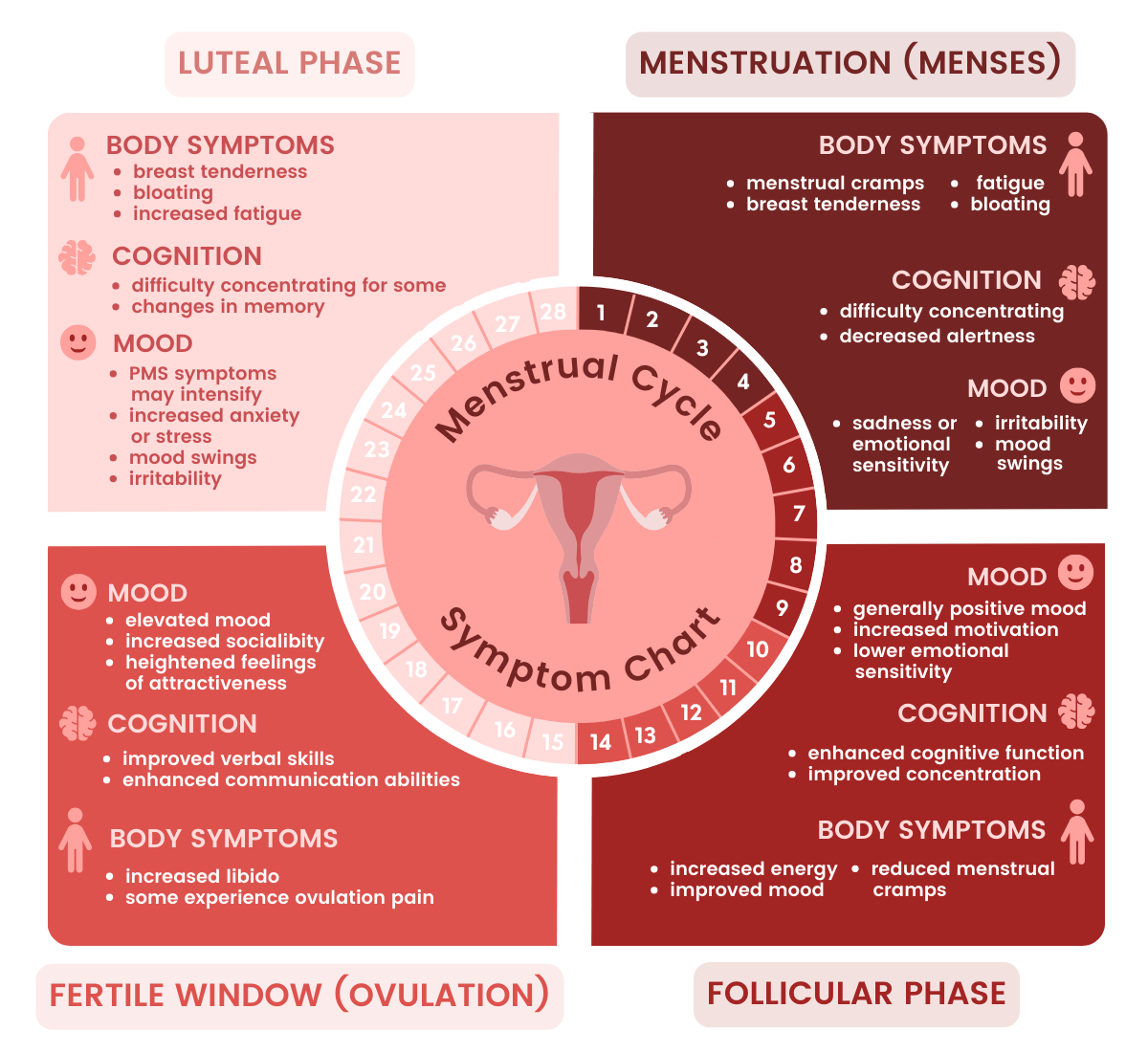
An infographic showing common symptoms associated with each phase of the menstrual cycle.
Because brain and hormone changes could affect the whole body, one might consider how these changes inform other health areas. Changes in executive functioning and other menstrual symptoms may influence daily activities and health goals — including exercise.
Cycle-dependent exercise routines are a trendy topic on social media. The impact of brain changes and hormonal changes on motivation, visual and spatial perception, social media accounts, and exercise programs may recommend specific exercises for certain cycle phases.
Here’s what Rizor had to say on the subject: “There are recommendations out there to do certain exercises during certain phases of your cycle, but there’s no one answer for everyone. It’s more about what works for you — except for the health basics, like drink[ing] water and sleep[ing]. But when it comes to exercise, it’s definitely more nuanced.”
Instead, Rizor recommended pairing baseline knowledge of your biology with tuning in to your body’s signals. This can help you gauge what movement you’re actually craving, instead of disconnecting more by adhering to strict and generalized fitness routines.
“If you have this understanding of the cycle as a rhythm and pulse cascading throughout your whole body, affecting your brain and many different areas, then you can be more understanding and kind to yourself that you might want to tweak your routine,” Rizor said.
Conclusion
With all of the conflicting health information available online — it’s easy to get lost and confused about what to do. What Rizor and her fellow researchers at UCSB are discovering is that women have natural biological fluctuations. These fluctuations may correlate with differences in how women’s bodies feel throughout the month. Instead of continuing to disconnect and place generalized expectations on yourself, tune back in and give your body what it actually needs — a listening ear and response to its signals.
This story was produced by Guava Health and reviewed and distributed by Stacker Media.