HIV isn't the death sentence it once was: How related deaths are dropping in the US
Photo Illustration by Elizabeth Ciano // Stacker // Shutterstock
HIV isn’t the death sentence it once was: How related deaths are dropping in the US
Hand holding AIDS awareness ribbon with HIV self test and treatment pill.
More than 1 million Americans live with human immunodeficiency virus, or HIV, with tens of thousands of new diagnoses each year. But with earlier diagnoses and advances in treatment, HIV, the virus that causes AIDS, has become far more manageable. Death rates among diagnosed individuals have dropped, even as recently as the past five years.
Stacker analyzed data from the Centers for Disease Control and Prevention to better understand drops in HIV-related deaths nationally and among certain subpopulations, taking a closer look at the factors behind these declines.
Overall, the CDC reports that 4,145 people died of a known cause related to HIV in 2022, a drop of about 19%—or 971 fewer deaths—compared to 2018. Dr. Robyn Neblett Fanfair, director of the HIV prevention division at the CDC, said this is due to ever-evolving HIV testing and treatments.
“HIV testing is becoming more of an option as people seek care, wherever they seek care,” Fanfair told Stacker. “That’s in community-based organizations, their primary care settings, family planning settings. It’s been wonderful to see HIV tests become a part of overall well-being and health care in this country.”
A hallmark of modern HIV treatment is viral suppression, or reducing the presence of HIV in one’s blood to very low levels, which keeps patients healthy and prevents transmission. Nearly 2 in 3 Americans diagnosed with HIV have reached viral suppression, though the lowest rates are among women, those aged 25 to 34, Black people, and people who inject drugs, Fanfair said. New efforts in testing, treatment, and prevention are particularly targeted at these and other disproportionally affected groups.
Fanfair highlighted one recent testing innovation, Together TakeMeHome, a program for HIV self-tests that people can order via delivery. Demand for the tests was beyond what Fanfair’s division anticipated, showing real eagerness for self-initiated testing among Americans, she said.
HIV treatments have also advanced substantially. In the past few years, researchers have developed combination pills so that those with HIV may only have to take one pill per day, rather than the dozens of daily pills characteristic of earlier antiretroviral treatments. Recently released treatments also include long-lasting injections, which patients only receive every few weeks or months.
Fanfair, who is also a medical provider for people living with HIV, called both innovations “revolutionary.” She said other modalities are continuing to come out as well, giving HIV patients myriad treatment options that help them to live long and healthy lives.
“What these promising declines of HIV-related deaths really show us is the power of ongoing HIV care and treatment in this country,” she said.
You may also like: As the US population ages, these states have the most older residents
![]()
Stacker
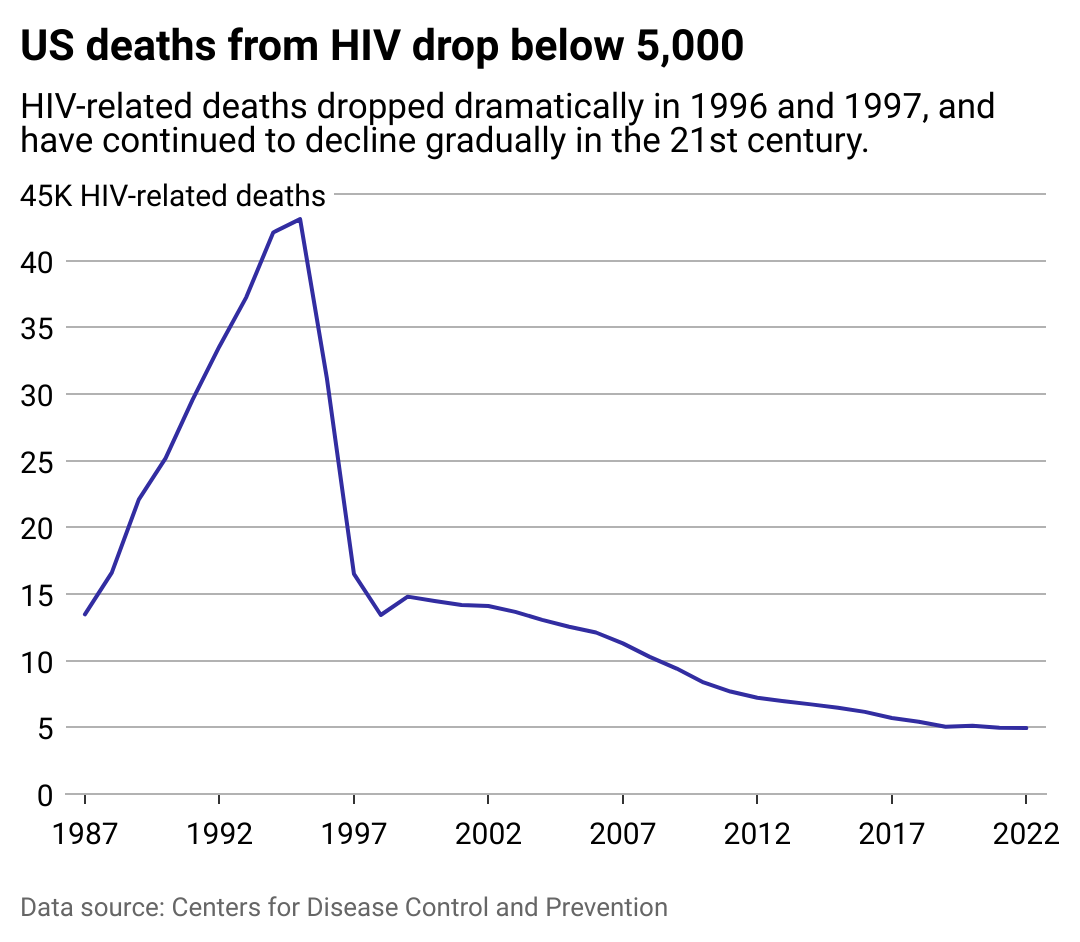
HIV deaths continue to fall in 21st century
A line chart showing HIV-related deaths over time. Deaths peaked in 1995, then dropped dramatically in 1996 and 1997, and have continued to gradually fall in the 21st century.
It took decades to reach current strides in HIV care, largely due to early public health failures.
The first U.S. cases of AIDS emerged in 1981, though health officials at the time didn’t yet fully understand the disease or its implications. It was first identified as a “gay cancer” as it mainly affected gay men and was associated with Kaposi’s sarcoma, a rare form of cancer linked to weakened immunity. It further spread among other marginalized communities, namely intravenous drug users, immigrants, and communities of color; as a result, the disease was largely overlooked by policymakers and public health officials. Those with the disease and those attempting to treat them faced rampant discrimination.
Lacking proper funding, research, and resources, the disease spread quickly and was incredibly deadly. By the end of that first year, there were 337 reported cases of individuals with severe immune deficiency, and nearly 2 in 5 had already died. The life expectancy for those diagnosed with HIV or AIDS was just one or two years.
It took outcry from affected communities, medical professionals, and activists before the U.S. and international health community took major action to combat the growing epidemic. The first public AIDS research and treatment was funded in 1983—two years after initial reports. In the interim, research remained limited, and dangerous misconceptions took root about the disease and how it spread. Not until the mid-’80s was it understood that HIV spread through bodily fluids like blood, semen, vaginal fluid, and breast milk, but not through casual contact or other bodily fluids like saliva. Even then, as stigma and discrimination persisted, deaths surged.
AIDS was the leading cause of death for American men between the ages of 25 to 44 in 1992, and two years later it became the leading cause of death for all Americans in that age bracket. By 1996 death rates had dropped, though remained the leading cause of death for Black Americans.
When highly active antiretroviral therapies were introduced to treat HIV in the late ’90s and early 2000s, the disparity in mortality rates grew between white and Black HIV patients. Studies suggest that this was due to fewer medical professionals providing these advanced treatments to Black populations and government policies limiting care in low-income communities, on top of other social factors.
Decades later, racial disparities persist in HIV infections and deaths. This is especially true among Black populations, namely Black women, youth, gay and bisexual men, and Black populations in the South. Although they only account for 12% of the population, Black Americans make up 39% of new HIV diagnoses, 40% of people living with HIV, and 43% of HIV-related deaths. Stigma and discrimination, higher poverty rates, lack of health care access, and less awareness of HIV status contribute to these ongoing disparities.
Stacker
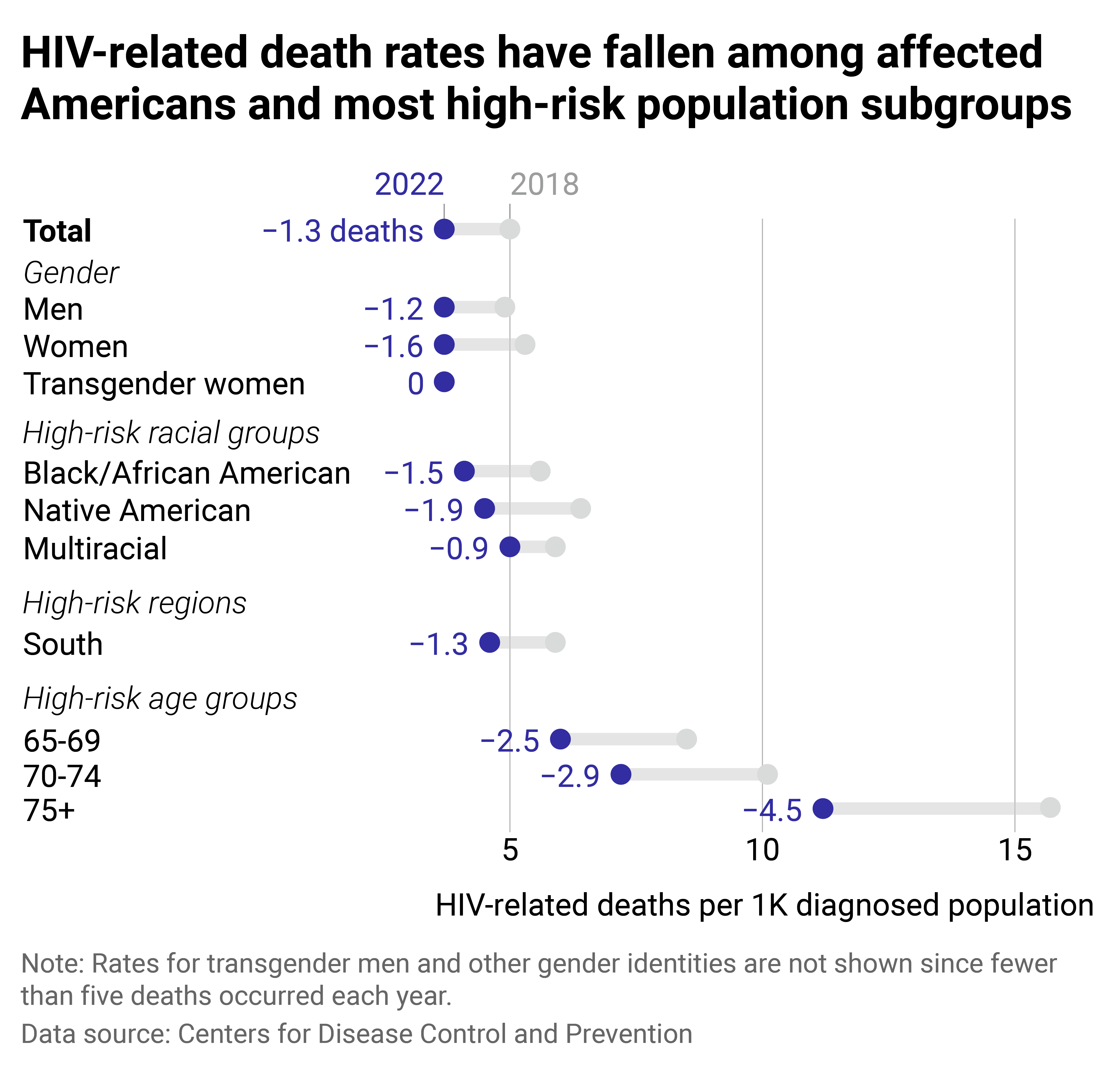
Death rates fell among highly affected HIV subpopulations
A range chart showing the death rates for HIV-diagnosed subpopulations in 2018 and 2022. Most populations included saw HIV-related death rates decline, except for transgender women, whose HIV-related death rates remained constant.
Medical breakthroughs have reduced death rates for Americans with HIV, including groups that are disproportionately affected by the virus. Even in the past five years, HIV-related death rates fell for all diagnosed Americans and across most at-risk groups.
Some of the largest drops have been measured among older people. Three decades ago, growing old with HIV wasn’t a likely outcome—in the 1980s, the life expectancy was just three years after diagnosis for people living with AIDS. But as effective treatments have allowed people to lead long and healthy lives, aging with HIV has become a major focus for researchers. As of 2023, life expectancies for most people receiving HIV treatment was about the same as the overall population. Those aging with HIV have similar health concerns to other aging Americans but remain at higher risk for some HIV-associated conditions like cardiovascular disease, diabetes, renal disease, and cancer.
HIV-related death rates also dropped among Black, multiracial, Hispanic or Latino, and Native American or Alaska Native populations. Rates remained consistent among transgender women and girls, though their actual number of HIV-related deaths rose from 2018 to 2022.
Some disproportionately affected populations have been prioritized in the White House’s 2021 HIV/AIDS strategy, which puts forth a roadmap to end the U.S. HIV epidemic by 2030. The document provided guidelines to achieve this goal, including improving health outcomes for those with HIV and reducing related disparities and health inequities. Hundreds of millions of dollars have gone toward these goals over the past few years, funding health centers, treatment access, workforce training, and other resources.
Much funding and support is targeted at specific communities where new infections have been highly concentrated. This often means supporting work at the local or community level to ensure that people can access HIV care in the places where they already go for health and other services, Fanfair explained.
Federal funding aimed at reducing disparities has proven effective in the past, particularly in decreasing HIV-related death rates for Black and Hispanic populations, according to a 2020 study. Today’s falling death rates indicate that the same may be true of these more recent efforts toward overburdened communities.
The combination of federal attention, medical advancements, and outreach in affected communities has led to great improvements in American HIV care. Moving forward, researchers are pursuing preventative vaccines and cures. In addition, the National Institute of Allergy and Infectious Diseases is looking at intersections with other diseases, expediting small and early-stage trials, and working to ensure that research is accessible to and representative of the most affected populations.
“Thinking of ways that we can support access to all communities is going to be really critical,” Fanfair said.
Story editing by Alizah Salario. Copy editing by Tim Bruns.
