How hospital employment has changed in 20 major metros

Canva
How hospital employment has changed in 20 major metros
A closeup of surgeons in an operating room performing a surgery.
Hospitals have added more than half a million jobs nationwide over the past decade. Just in the past year, hospital employment grew by 152,000, or about 3%, Bureau of Labor Statistics data shows. The U.S. population is growing and aging, and people are living longer. As a result, health care jobs—including those at hospitals—are expected to grow at above-average rates.
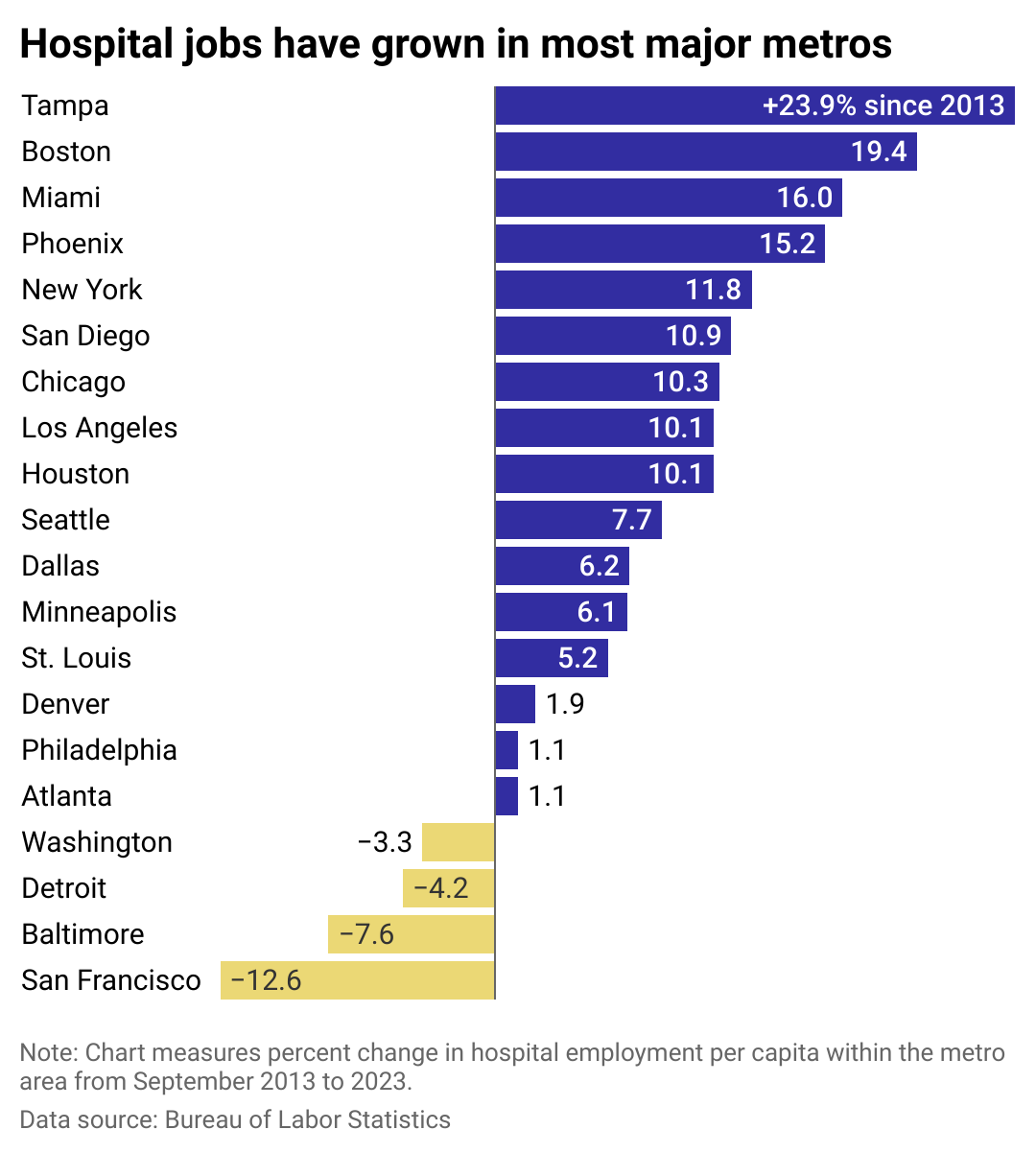
Medical Technology Schools used Bureau of Labor Statistics data to see how employment at hospitals has changed among 20 major U.S. metros in recent years and what has contributed to some of those trends. Most metros saw sizable increases in hospital workers per capita over the past 10 years. However, a few saw those ratios decrease amid a shortage of doctors, nurses, and other medical professionals.
U.S. health facilities may struggle to fill jobs vacated by retirees and career switchers, let alone find professionals to fill new roles. Health care providers are experiencing increased burnout, and some hospitals—particularly in rural areas—face funding challenges. Still, in addition to per capita figures, overall hospital employment grew in all but four of the metros included in the analysis.
This analysis uses metropolitan statistical areas for most cities, but due to data availability uses metropolitan divisions (subdivisions of metropolitan areas) in a few cases: New York, Los Angeles, Chicago, Washington D.C., and San Francisco. Base data are not seasonally adjusted.
![]()
Medical Technology Schools
Most metros have added hospital staff
A bar chart showing the percent change in hospital employment from 2013 to 2023 within 20 major metros.
By volume and per capita, most metros have grown their hospital staffs.
Tampa led the cohort in hospital growth per capita. The metro’s population is growing incredibly fast, and its hospitals have followed suit. In addition to a budding Medical and Research District, the region’s leading Tampa General Hospital is expanding rapidly. Last year, Tampa General opened a new rehabilitation hospital, and now it’s in the midst of a 500,000-square-foot hospital expansion that will create nearly 6,000 jobs.
Tampa isn’t the only part of the Sunshine State with an abundance of hospitals—and for good reason. In 2019, Florida eliminated government approval requirements for new hospitals. Now, dozens of them are going up across the fast-growing state. While ease of access for many residents may improve, KFF Health News reported that having more hospitals could end up escalating health care costs.
That’s what led Massachusetts to block some hospital additions in Boston, where government approval is still required. Despite a few rejections and repeals, several hospitals throughout the metro are building capacity, including Brigham and Women’s Faulkner Hospital, Boston Children’s Hospital, Massachusetts General Hospital, and Beth Israel Deaconess Medical Center.
The COVID-19 pandemic stressed Boston’s existing hospital infrastructure, adding urgency to upgrade and add hospital beds throughout the city. Boston is an international hub for medicine and life sciences, so it’s unsurprising for it to be among the metros leading the country in hospital employment gains.
Not every metro is experiencing the same surplus. Hospitals in San Francisco—and across California—have faced consolidations and closures due to financial and staffing challenges. Dr. Renee Hsia, a professor at the University of California San Francisco’s Department of Emergency Medicine, told the San Francisco Chronicle that health care services are often reduced in areas where private insurers aren’t footing the bill (i.e., where Medicare and Medicaid are more prevalent). In turn, remaining hospital resources are strained: Emergency room wait times and crowding have increased, often forcing ambulances to be rerouted to another facility due to a lack of hospital beds.
Hospitals in Maryland are facing more acute staffing shortages, particularly among nurses. A 2022 report found that 1 in 4 of the state’s nursing positions was vacant, with the highest vacancy rates among the Baltimore and Washington D.C. metro areas. In addition to the nursing shortages plaguing the country, Maryland is also in the midst of a backlog of license approvals and renewals, exacerbating the situation and keeping travel nurses from entering the equation.
In Maryland and other parts of the country, attempts to close the staffing gaps are being made with higher pay for medical workers, increasing health care visas, new medical schools, tuition reimbursement programs, and stronger job placement pipelines.
Story editing by Ashleigh Graf. Copy editing by Tim Bruns.
This story originally appeared on Medical Technology Schools and was produced and
distributed in partnership with Stacker Studio.