‘A difficult situation’: St. Charles gives details of hospitals in crisis at community town hall
(Update: Adding video, comments)
Issues are many -- and far from unique; National Guard help sought, county mask mandate urged
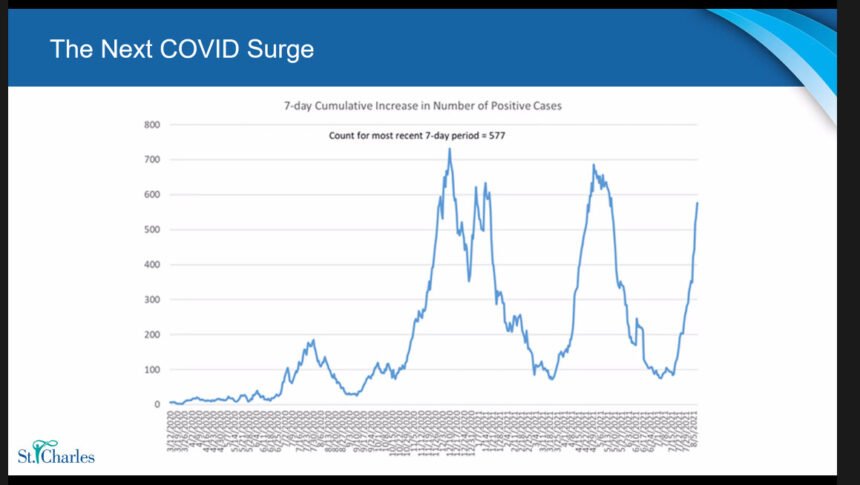
BEND, Ore. (KTVZ) – St. Charles Health System detailed a worrisome set of statistics and facts at an online town hall Tuesday to underscore the crisis facing its four hospitals as the COVID-19 delta variant, twice as contagious as the initial virus, sends cases soaring and makes for an even more complex, uncertain path toward solutions.
“What we’re seeing month after month since the pandemic has begun is we’re running at max capacity pretty much every day -- and when we’re not, we’re starting the day at 90-95% occupancy,” said Aaron Adams, president of the St. Charles Health System.
Stressing that the situation in Central Oregon is far from unique in Oregon or the country, hospital officials said they have requested Oregon National Guard assistance and are joining others in urging Deschutes County to impose an indoor mask mandate – a situation the state may soon make moot.
“There is no way to sugar-coat it: We are in a difficult situation,” Adams said. A recording of the town hall is available on the health system's Facebook page.
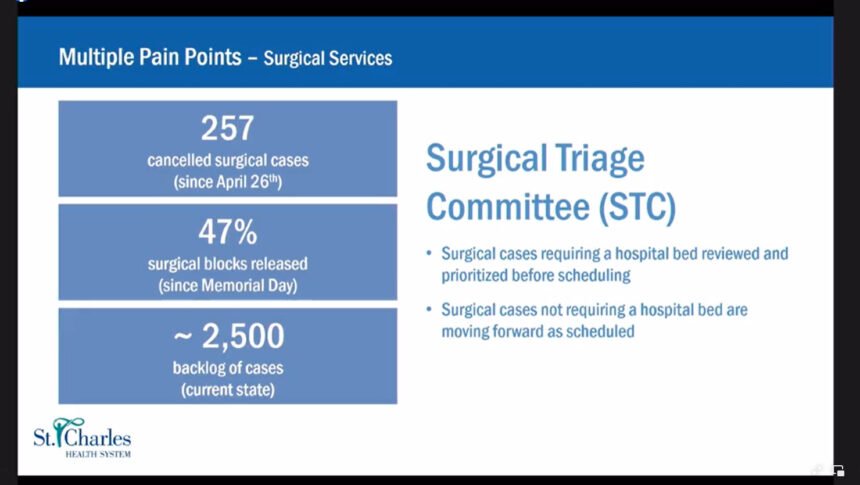
More than 250 non-urgent surgeries have been canceled since late April and there is a backlog of 2,500 cases, meaning some patients have been waiting “well over a year” for needed procedures, said Dr. Douglas Merrill, chief medical officer, as he noted the “multiple pain points” the hospitals are facing.
A surgical triage committee has been set up to review and prioritize surgeries that require a hospital bend – others, that don’t require patient admittance, are moving forward as scheduled, he said.
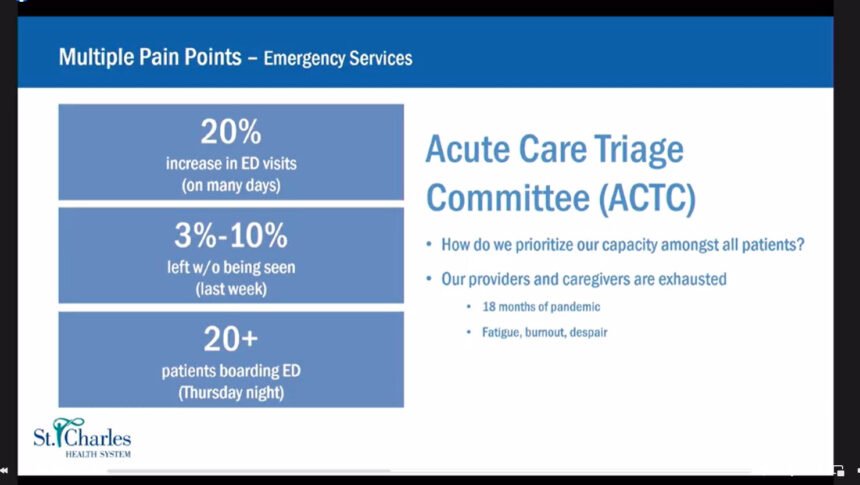
Emergency rooms are “extraordinarily busy” this year, Merrill said, seeing a 20% increase from a year ago on many days, largely “due to patients not having been able to get in to have chronic diseases managed.”
A range of 3-10% leave without being seen, and there were 20-plus patients boarding in the Emergency Department Thursday night, waiting for a hospital bed.
The workload is putting a strain on all: “Our providers and caregivers are exhausted,” Merrill said, suffering “pandemic fatigue” after 18 months, with “burnout and despair” also listed on the slide presentation. They are “despairing of a light at the end of the tunnel,” he added, in part due to the “sizable number of folks not vaccinated,” a situation common across the country.
Adams added, “Asking this group to manage a full hospital every day, asking people to continuously pick up extra shifts, to work extended hours, month after month after month, is not really a sustainable model.”
Hospitals are seeing that the delta variant of the virus is “beginning to affect kids far more than it did,” and staffing shortages mean adults are “having to go hours away for a hospital bed.”
Adams said the system’s hospital beds are at maximum capacity every day, and there are at present 125 open RN positions in Bend, with 61 on leave or lighter duty, nearly a third of that workforce, so others pick up extra shifts or work longer hours “month after month.”
“Our folks have been heroic in the way they’ve responded, rallied to care for patients, but it’s not something we can rely on indefinitely,” Adams said, adding that they must seek to “surge up” staff beyond the current hospital capacity.
“We’re going to see more turnover, if we’re not going to be able to get these folks help,” Adams said, noting the problems all businesses in a hiring squeeze also face, such as lack of affordable housing and available child care.
More troubling statistics: a 25% increase in the number of traumas seen, compared to 2019, and up 40% from last year.
Another big challenge is hospital discharges, with stays averaging five days now, up a full day (20%) from 2019.
“People are sicker,” Adams said, and those infected by COVID are staying in hospitals longer. On Friday, they were 42 patients in the hospital solely because they were waiting for beds elsewhere, such as a skilled nursing, assisted living or memory care facility – all part of the “continuum of care” elements that depend on each other.
Dr. Cynthia Maree, the hospitals’ medical director of infectious disease, noted that skilled nursing facilities must close for at least two weeks, if an outbreak occurs. But she said the vaccines are still proving very effective at protecting against severe disease and hospitalization, though they are seeing more “breakthrough” cases.
Maree said 76% of St. Charles caregivers are vaccinated, as the hospital system works toward the Sept. 30 state deadline that will require staff to provide proof of vaccination or get weekly COVID testing.
Julie Ostrom, senior director of perioperative and cardiovascular services, said the plan through the end of the year is to not schedule elective surgeries until they are reviewed and prioritized, to try to cut down on frustrating, repeated cancellations.
During questions from reporters, Dr. Jeff Absalon, chief physician executive, said St. Charles has asked Deschutes County commissioners to again consider a masking mandate for indoor communities, also asking the Bend and Redmond city councils. “It’s very important we have people do the masking as much as absolutely possible,” he said.
He also said, “We have asked for National Guard help, but a shortage of nursing staff is our predominant issue,” and nursing staff available from the Guard is “limited and working in other locations.” But they are going through the process for help from other Guard resources, also asking the state to possibly increase to a Level 3 incident command structure, to help better allocate needed and available resources.
And hospital officials offered a familiar set of ways the community can help – above all to get vaccinated, but also to wear a mask indoors, see your doctor when necessary, practice good self-care, don’t delay care and choose the right place to be seen.
The “impact on patients is troubling,” Adams said. “It’s not the type of care anybody wants to provide. It’s not the fault of the surgeons, or the office staff. It’s just unfortunate circumstances we find ourselves in,” and are working to address in various ways.
In the meantime, Ostrom said, if an emergency surgery is needed, it’ll happen: “Part of what we’re doing with capacity is managing elective surgery, to maintain the ability for those who arrive with urgent, emergency needs."